Introduction: Choosing a suitable donor is essential to achieve a good response for allogeneic hematopoietic cell transplantation (allo-HCT). Several previous studies have compared unrelated bone marrow transplantation (UR-BMT) and cord blood transplantation (CBT), but the results differed among each study, and their superiority has been controversial. The total number of nucleated cells (TNC) in cord blood unit is crucial for CBT to avoid early complications, including engraftment failure. The outcome of CBT may improve by choosing cord blood unit with a higher TNC.
Methods: We retrospectively compared the outcomes of CBT with higher TNC (hCBT) and UR-BMT conducted in our institute from January 1st, 2013, to May 31st, 2023. Cut off point of TNC was the median value. The primary endpoint was overall survival (OS), and the secondary endpoints were non-relapse mortality (NRM), cumulative incidence of relapse, and cumulative incidence of complications.
Results: We analyzed a total of 316 patients, including 139 patients who underwent CBT and 177 patients who received UR-BMT. The median infused TNC was 2.71 (range, 0.027-6.42) ×10^7/kg. hCBT group included 69 patients.
Significantly more patients in the hCBT group had prior allo-HCTs (hCBT: 18.8%, UR-BMT: 5.6%, p=0.003), and hCBT procedures were more frequently conducted since 2018 (hCBT: 66.7%, UR-BMT: 36.7%, p<0.001). For each group, most patients received tacrolimus and short-term methotrexate as graft-versus-host disease prophylaxis (hCBT: 94.2%, UR-BMT: 95.5%, p=0.277). ABO matched donors were more commonly chosen for UR-BMT (hCBT: 24.6%, UR-BMT: 46.3%, p=0.006). Patients with myelodysplastic syndrome underwent UR-BMT more frequently (hCBT: 7.2%, UR-BMT: 20.9%). Patients with a high or very high disease risk index were more frequently included in the hCBT group (hCBT: 37.5%, UR-BMT: 27.9%, p=0.060). Patient sex, age, days from diagnosis to transplantation, and hematopoietic cell transplantation comorbidity index, conditioning intensity were well balanced between each group.
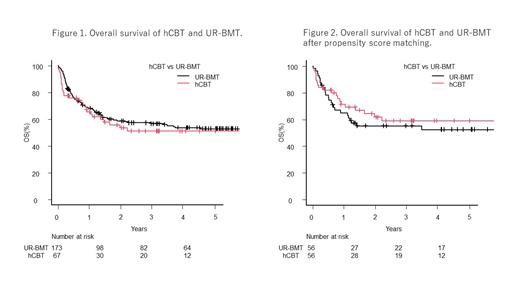
The two-year OS of hCBT was equivalent to UR-BMT (hCBT: 53.6%, UR-BMT: 58.9%, p=0.56) (Figure 1). There was no significant difference in the two-year NRM between the two groups (hCBT: 24.9%, UR-BMT: 25.4%, p=0.87). The hCBT group had a lower neutrophil engraftment rate achieved at day 28 (hCBT: 83.0%, UR-BMT: 92.3%, p<0.001). The two-year relapse rate was similar between the hCBT and UR-BMT groups (hCBT: 26.1%, UR-BMT: 18.7%, p=0.34). The cumulative incidence of acute GVHD tended to be lower in the hCBT group (hCBT: 18.2%, UR-BMT: 33.6% at 100 days, p=0.067), and the same results were observed when analyzing grade 2-4 or grade 3-4 acute GVHD. The cumulative incidence of chronic GVHD was significantly lower in the hCBT group (hCBT: 4.7%, UR-BMT: 48.3%, p<0.001), and the cumulative incidence of severe chronic GVHD was also lower in hCBT group (hCBT: 0.0%, UR-BMT: 13.9%, p<0.001).
To reduce the impact of patients' characteristics, propensity score matching was conducted. The covariates included prior allo-HCTs, disease risk index, and allo-HCT conducted before 2018 or not. After propensity score matching, a total of 116 patients were included in the analysis with 58 patients for each group. The two-year OS of hCBT was also equivalent to UR-BMT (hCBT: 61.8%, UR-BMT: 55.2%, p=0.43) (Figure 2). The two-year NRM was slightly lower in hCBT group, but it is not significant (hCBT: 19.1%, UR-BMT: 30.1%, p=0.21). The hCBT group had a late neutrophil engraftment (hCBT: 87.0%, UR-BMT: 89.1% at day 28, p<0.001). The two-year relapse rate was similar between the hCBT and UR-BMT groups (hCBT: 25.0%, UR-BMT: 20.0%, p=0.54). The cumulative incidence of acute GVHD was tended to be lower in hCBT group (hCBT: 19.8%, UR-BMT: 38.7% at 100 days, p=0.057) and the cumulative incidence of chronic GVHD was significantly lower in hCBT group (hCBT: 5.3%, UR-BMT: 56.3%, p<0.001).
Discussion: This was the first study to validate that the outcomes of CBT with higher TNC were equivalent to UR-BMT. Although the hCBT group experienced later neutrophil engraftment, the rate of neutrophil engraftment achieved at day 28 was comparable to UR-BMT, and a lower incidence rate of chronic GVHD might be attributed to lower NRM. From these findings, hCBT may be a worth considering option for patients requiring allo-HCT.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal